INSIGHT New farm clinic newsletter - Summer Edition 2015
Welcome to the 4th edition of Insight.
We are delighted to welcome you to our quarterly newsletter, "Insight".
This quarterly publication focuses on you and your health care to ensure that your 'patient journey' at New Farm Clinic is a successful one.
Insight is a great way for starting a conversation about mental illness, health and wellness.
We want to make a real difference in the lives of those we treat.
Read personal accounts from lived experiences and positive professional information. We aim to reduce the stigma, raise awareness and understanding of all things about the mind.
To provide accurate and helpful information to everyday people on a range of health and social topics specifically related to mental health and wellness by using non-technical, non-clinical, supportive and easy to read articles.
We want to hear from you - let us know what you think of this newsletter - and what suggestions you have.
PLEASE FEEL FREE TO PASS THIS ON TO YOUR FRIENDS & CARERS. ENJOY THE NEWSLETTER, AND I HOPE TO SEE YOUR FEEDBACK IN THE NEAR FUTURE.
Mick Pullen - Assistant Director of Clinical Services

Development Update

New Farm Clinic, currently an 89 bed facility, is located in the leafy river suburb of New Farm in Brisbane. In 2016, New Farm Clinic will expand to 128 beds — all single rooms with ensuites. The redeveloped facility will include 10 consulting rooms in a purpose-built medical centre; a new car park; gymnasium and five group therapy rooms for patients. Construction is expected to be completed by October 2016 including the conversion of shared rooms in the existing facility to all private rooms.
Clinic CEO Ken Craig said the opening of these new contemporary mental health facilities would be welcomed by patients, staff and doctors.
"The new facilities will ensure that quality mental health care is now more accessible to people in Queensland with a mental illness,”

“Today, Brisbane is experiencing a growing demand for mental health services and New Farm Clinic is one of a few private mental health facilities providing services in the Brisbane area. The Clinic treats over 7000 patients each year and plays a significant role in the local community caring for people suffering with a mental illness.”
New Farm Clinic is a purpose-built mental health care facility that has been in its current location since 1986. In 2016 it will celebrate its 30th anniversary. The Clinic provides a number of critical services. It has a 10 bed inpatient eating disorder program, the only private inpatient eating disorder service in the State, and therefore provides an invaluable service to its patients and their parents or carers.
New Farm Clinic specialises in the management of depression and anxiety and runs both inpatient and day patient programs.
New Farm Clinic Group Therapy Day Programs
The objective of day programs is to deliver group therapy that provides patients with the skills and support to help improve the quality and enjoyment of life and break the cycle of relapse, and therefore the need for hospitalisation. The individual programs are designed to promote the use of effective coping strategies and a return to normal functioning.
Social Development
For individuals with limited social skills, intellectual impairment, or diagnoses such as schizophrenia.
Social Development is based on building social connections through structured activity such as puzzles, board games, and going out for coffee. Social development has no start or end date. Group members are encouraged to stay in the group until they no longer find it beneficial.
Cognitive Behaviour Therapy (CBT)
Ideal for individuals that struggle with anxiety and depression.
CBT is the leading recognised treatment for depression and anxiety. It involves strategies to help change unhelpful thinking patterns, as well as practical strategies to help change behaviour. The full course is a 10 week program but some benefit from attending the group for a number of rounds. Patients can enter the course at any time
Life Skills
Life Skills was originally designed for individuals who have completed the CBT program and would benefit from ongoing support.
Life Skills is a support group that addresses topical areas of ongoing recovery of mental health, such as relationships, assertiveness, emotions etc. Life Skills has no start or end date. Group members stay in until they feel ready to graduate.
Dialectical Behaviour Therapy (DBT)
DBT was originally designed for individuals with personality disorders, but is now recognised as beneficial for a number of mental health issues including Complex Post Traumatic Stress Disorder, impulsivity, anger and emotional regulation and self-harm behaviours. DBT is particularly useful for suicidality and self-harm, or for individuals with complex mental health issues that require more intensive intervention and support. DBT requires an assessment with a DBT group facilitator.
DBT is a group that primarily aims to address individuals that greatly struggle with balancing their emotions. It includes four topics: Mindfulness (being in the present moment), Distress Tolerance (coping with crisis and overwhelming feelings), Emotion Regulation (skills to balance emotions), and Interpersonal Effectiveness (relationship skills). DBT involves weekly homework to practice the skills.
Minimum of 6 months commitment is required, but attending 2 or 3 rounds is recommended in order to have fully established the skills.
Dialectical Behaviour Therapy for Young Adults
Individuals ages 18-25 years.
The same content & patient commitment is required as detailed above for DBT.
Advanced Dialectical Behaviour Therapy
Individuals who have graduated from the New Farm Clinic DBT program but would like continued support to prevent relapse.
Focuses on encouraging group members to continue to utilise and implement their DBT skills to assist them to apply their skills to more complex problems.
Minimum commitment of 3 months.
Eating Disorder Group – Mind Body Therapy (MBT)
MBT is for individuals whose primary struggle is binge eating. MBT requires an assessment with a MBT group facilitator.
MBT involves strategies to manage binge eating and as well as skills to balance emotions. Morning tea and lunch from the New Farm Clinic dining room are part of the program.
Minimum of 2 months commitment, with progress being reviewed every 6 months.
Eating Disorder Group – The Therapeutic Anorexia Nervosa Support Group (TANS)
TANS is for individuals whose primary struggle is restrictive eating, but individuals may also struggle with other eating disorder behaviours such as over exercising. TANS requires an assessment with a TANS group facilitator.
TANS involves strategies to address under eating and other eating disordered behaviours. It also focuses on identifying the issues that underlie eating disorder behaviours. Morning tea and lunch from the New Farm Clinic dining room are part of the program and must be fully completed.
Minimum of 2 months commitment, but group members are encouraged to stay in the group until they are ready to graduate.
Meet the team - Allied Health

Senior Clinical Therapist Day Program Facilitator: Life Skills and Advanced Dialectical Behavioural Therapy Registered, Credentialed Mental Health Nurse with Masters in Counselling.
Specialised training: REBT through the Institute of Rational Emotive Therapy and The Linehan Institute Behavioural TECH Dialectical Behavioural Therapy training, Mentalizing Based Treatment.

Day Program Facilitator: Dialectical Behavioural Therapy B.A. (Hons) MClinPsych G COrgPsych MAPS.
Specialised training: Dialectical Behaviour Therapy, Schema Therapy and The Linehan Institute Behavioural TECH Dialectical Behavioural Therapy training.

Day Program Facilitator: Dialectical Behavioural Therapy (DBT) BSc, Diploma in Counselling, MA in Psychotherapy Studies.
Specialised training: Four year training in Psychoanalytic Psychotherapy, Advanced Mentalizing Based Treatment Practitioner Training and The Linehan Institute Behavioural TECH Dialectical Behavioural Therapy training.

Day Program Facilitator: Mind & Body Therapy – Binge Eating, Cognitive Behaviour Therapy and Life Skills BSc PG Dip Psych.
Specialised training: Schema therapy, Cognitive Behaviour Therapy, Suicide Prevention, The Linehan Institute Behavioural TECH Dialectical Behavioural Therapy training. Currently undertaking STAP training.

Inpatient Therapist: Cognitive Behaviour Therapy Day Program Facilitator: BA Soc. Wrk. AMHSW.
Specialised training: Dialectical Behavioural Therapy, Cognitive Behaviour Therapy, Systemic Family Therapy, NLP, Conflict resolution, Workplace Trainer, Accidental First Aid, Aggressive behaviour and Suicidal and Intervention Counsellor.

Day Program Facilitator: 18 – 25 Dialectical Behaviour Therapy BA Psych, PG Dip Psych.
Specialised training: The Linehan Institute Behavioural Tech Dialectical Behavioural Therapy training Acceptance and Commitment Therapy.

Day Program Facilitator: Advanced Dialectical Behavioural Therapy Master Applied Psychology (Counselling Psychology); Doctorate Clinical Psychology (Candidate).
Specialised training: The Linehan Institute BehavioralTECH Dialectical Behavioural Therapy training, Psychodynamic, Acceptance and Commitment Therapy, Cognitive Behaviour Therapy, Dialectical Behavioural Therapy and STAP accredited Supervisor.

Inpatient Therapist: Cognitive Behaviour Therapy and Dialectical Behavioural Therapy Day Program Facilitator: Mind & Body Therapy – Binge Eating BA Psych (Hons) .
Specialised training: Cognitive Behaviour Therapy, Cognitive Behaviour Therapy for Eating Disorders, Acceptance and Commitment Therapy and The Linehan Institute Behavioural TECH Dialectical Behavioural Therapy training.

Day Program Facilitator: 18-25 Dialectical Behavioural Therapy and Dialectical Behavioural Therapy B.BehSc. GradDipPsych. Mpsych(Org).
Specialised training: The Linehan Institute Behavioural TECH Dialectical Behavioural Therapy training, Cognitive Behaviour training, Acceptance and Commitment Therapy and Schema Therapy training.

Inpatient Therapist: Cognitive Behaviour Therapy and Dialectical Behavioural Therapy Day Program Facilitator: Therapeutic Anorexia Nervosa Support Group BA Psych and Post Grad Dip Psych .
Specialised training: Cognitive Behaviour Therapy, Cognitive Behaviour Therapy for Eating Disorders, Mindfulness and The Linehan Institute Behavioural TECH Dialectical Behavioural Therapy training.

Day Program Facilitator: Cognitive Behaviour Therapy and Dialectical Behavioural Therapy BA Psych .
Specialised training: Motivational Interviewing, Mentalisation Based Therapy, Acceptance and Commitment Therapy, Cognitive Behaviour Therapy, Mindfulness Based Therapy, Psychodynamic Psychotherapy, Interpersonal Psychotherapy and The Linehan Institute Behavioural TECH Dialectical Behavioural Therapy training.

Inpatient Therapist: Cognitive Behaviour Therapy and Dialectical Behavioural Therapy Day Program Facilitator: Therapeutic Anorexia Nervosa Support Group BSc (Hons), MClinPsych .
Specialised training: IPT training and The Linehan Institute Behavioural TECH Dialectical Behavioural Therapy training.

Day Program Facilitator: Social Development, BSc Psych, PG Dip Counselling & Behaviour Management, Master of Counselling .
Specialised training: Cognitive Behaviour Therapy, Introduction to Art Therapy, Cognitive Behaviour Therapy and The Linehan Institute Behavioural TECH Dialectical Behavioural Therapy training.
If you have any questions regarding any of New farm Clinic's Group Therapy day Program services please contact Jo Tan on Ph (07) 3254 9120 or email enquiries.nfc@ramsayhealthcare.com.au.
New Farm Clinic launches Facebook page
Follow Us on Facebook
Like Us on Facebook
Facebook boosts suicide prevention support for Australian users.
Facebook joins with leading Australian mental health groups to roll out a range of new suicide prevention tools to Australian social media users.
Facebook will be asking users to contact local emergency services if they see anyone posting a threat of suicide.
Mental health experts will prioritise the most serious reports, such as self-injury, and send help and resources to those in distress.
People posting about suicide will also be encouraged to connect to mental health specialists and reach out to friends.
The initiative follows similar tools launched by Facebook in the US.
Anyone who alerts Facebook about a post regarding suicide will also receive support
CEO puts himself in staff shoes

With New farm Clinic's major redevelopment underway Clinic CEO Ken Craig wanted to gain a better understanding of what it's like to do many of the jobs that are vital to how the clinic operates.
"I wanted to see the challenges our team face during their daily work routine & gain 'hands' on experience by working alongside them".
Working with & alongside staff provided Ken with an excellent opportunity to listen to their innovative ideas on how the clinic could improve its operational efficiencies & resulted in constructive changes to policies & procedures, which may have otherwise been missed opportunities.
"The overall experience allowed me to connect directly with team members to gain intimate knowledge of their jobs & to develop a better appreciation of their commitment & contributions".
"This opportunity has allowed me to see first hand the excellent teamwork, dedication & pride each team member takes in doing their job".

Eating Disorders
Eating disorders are a major public health problem and blight the lives of young people and their families. Not all sufferers with eating disorders are young and/or underweight. Eating disorders affect males and females of all ages and all walks of life. They often, but not always, begin around puberty however it may be several years into the disorder before sufferers realise the extent of the problem. Most sufferers change between diagnoses over time as their situations change.

Eating disorders fall into four categories:
- Anorexia Nervosa - This is a severe emotional disorder that impacts on the mind and damages the body through starvation. It is the third most chronic illness for adolescent girls in Australia (behind obesity and asthma).
- Bulimia NervosaThis is characterised by frequent episodes of binge eating followed by purging behaviours such as vomiting, laxatives, diuretics or excessive exercise in a frantic effort to lose weight.
- EDNOS (Eating Disorder Not Otherwise Specified) - This is where sufferers’ individual symptoms do not fit the criteria for either Anorexia or Bulimia. Sufferers’ symptoms are any mixture of the above criteria.
- Binge Eating Disorder - This is characterised by compulsive overeating with no attempt to avoid weight gain. The exact cause of eating disorders is uncertain, however a number of characteristics are commonly found in those who develop the disorder:
- Psychological factors such as low self-esteem, anxiety, self-criticism and perfectionism.
- Changes in life circumstances for example breakdown in relationships, trauma, abuse and neglect.
- Biological factors such as hormonal or chemical imbalances may also play a role in the development of an eating disorder.
There are two intense treatment options and both involve developing adaptive ways of coping to replace the maladaptive coping strategies developed with the eating disorder.
For many a 4-8 week inpatient stay is necessary to ensure medical and nutritional stability and provide education around ways to control the eating disordered headspace and to support behavioural changes: Day Programs are beneficial in long term support as they focus on improving sufferers coping skills and challenging eating disorder thinking.
Recovery may be a long and slow process that can involve relapse and readmission as part of the process.
Where Can I Find Help?
If you think you may need help, your GP is the best person to talk to in the first instance. Your GP will have information about local services which may be able to help. Your practice nurse or health visitor, who is based at your GP practice may also be able to help.
New Farm Clinic offers & provides a number of services and programs appropriate in the management of Eating Disorders. For information please contact our Assistant Director of Clinical Services or Day Patient Program Coordinator on (07) 3254 9100 or email.
Record Paul Ramsay Foundation grant to cut suicide
We are pleased to announce that the Paul Ramsay Foundation had engaged in a six year partnership with The Black Dog Institute to tackle suicide prevention in Australia. Under the guidance of CEO Professor Helen Christensen and Chairman Peter Joseph, the Black Dog Institute have launched the implementation of a world first evidence based approach to suicide prevention.
We are extremely excited to partner with such a high quality organisation and to see the results of this collaborative mental health initiative.
Every year, over 2500 Australians die by suicide and a further 65000 make an attempt.
Today, we are honoured to announce that the Paul Ramsay Foundation have stepped in to financially support the initial implementation of a new, evidence-based approach to suicide prevention in Australia.
According to Prof Helen Christensen, Director of the Black Dog Institute and the NHMRC Centre for Excellence in Suicide Prevention, we have the knowledge to save thousands of lives and lead the world in suicide prevention activities.
“In partnership with experts and consumers, the National and NSW Mental Health Commissions have both strongly recommended the implementation of an evidence-based and community-focussed approach to suicide prevention.”
“We are extraordinarily grateful to the Paul Ramsay Foundation for acknowledging the strength of the evidence and the severity of the problem, and the to the NSW Mental Health Commission for facilitating the translation of international evidence into a suicide prevention framework.
The systems approach to suicide prevention involves the simultaneous implementation of nine key strategies that target suicide risk both through medical and social interventions.
Local management means services can be tailored to local needs and are coordinated within the community by primary healthcare providers, education system, emergency services, community groups and other stakeholders.
Sites will be selected on the basis of need and will be implemented in partnership with local Primary Health Networks and community organisations. The trial will commence in 2016.
It is estimated that the new evidence-based solution will reduce the Australian suicide rate by at least 20% in just a few years and also significantly improve the lives of those in distress.
“Their support, which represents the largest philanthropic donation ever given to suicide prevention activities in Australia, has the potential to change the way suicide prevention is addressed in Australia, opening the door for a nationally coordinated framework,” says Prof Christensen.
The NSW Mental Health Commission funded the development of the Proposed Suicide Prevention Framework for NSW, which recommended using the systems approach. It also supported the next phase of Professor Christensen’s work, evaluating the operational resources needed to roll out the systems approach to suicide prevention in small towns.
John Feneley, the NSW Mental Health Commissioner, said the persistently high suicide rate meant new initiatives were urgently needed.
“This extraordinary donation lets researchers kick-start an approach that the international evidence suggests has every chance of being highly effective,” Mr Feneley said.
“It is about combining things that are already known to work. What we don’t yet know is exactly how many deaths and suicide attempts we can prevent when we pursue all these proven elements together in a wraparound, community-based response.”
“Seed funding can be the impetus to get important projects off the ground quickly,” Mr Feneley said. “Through the Ramsay Foundation’s leadership this work can now move quickly to the next level.”
The $14.7million donation from the Paul Ramsay Foundation will be used to implement and evaluate this new approach over six years in four sites across NSW.
“We are delighted to be able to support such a high quality organisation as Black Dog Institute in what is an absolutely vital project – Both in terms of saving lives and drawing attention to what is an area of critical need,” says Simon Freeman, CEO of the Paul Ramsay Foundation.
“Our Board of Directors highlighted mental health as one of the key areas they wanted the foundation to focus on therefore it is truly fitting that this is the first major grant that we have awarded.”
NSW Minister for Mental Health, the Hon Pru Goward MP will formally launch this new approach at Black Dog Institute on Thursday 3rd December. Further information about the systems approach can be found here http://www.blackdoginstitute.org.au/public/research/suicideprevention.cfm
The $14.7 million is the first major grant from the Paul Ramsay Foundation since the healthcare magnate died from a heart attack last year, and left the bulk of his estate to the foundation.
Paul Ramsay AO, Chairman and founder of Ramsay Health Care, passed away on 1 May 2014 in his home town of Bowral, leaving a philanthropic bequest of more than $3 billion to charity.
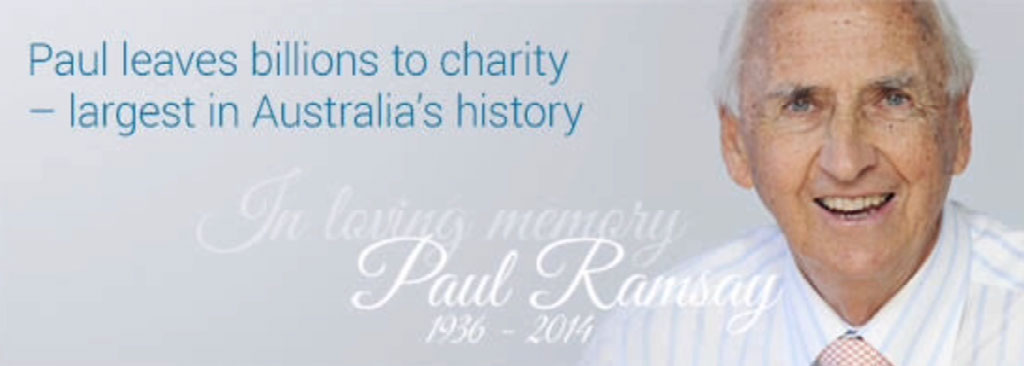
During his life, Mr Ramsay had been a generous benefactor to dozens of charities and worthy causes and in death, he has left the biggest single donation in Australia’s history to his personal foundation.

AUSTRALIA'S LEADING MENTAL HEALTH FACILITY NETWORK
Ramsay Health Care is the largest provider of private mental health services in Australia. With 21 hospitals and clinics around the country, we have expertise in mood disorders, drug and alcohol dependence, postnatal depression, eating disorders, post-traumatic stress disorder, and general mental health disorders.
We embrace The Ramsay Way culture, which recognizes that people – our staff and doctors – are our most important asset. Offering support services, rehabilitation, and other mental health treatment plans, our psychiatric clinics are equipped to help you.
If you believe that you or a loved one may need help, go to the locations page to see our mental health facilities and the treatments provided at each one.
NEW FARM CLINIC 22 SARGENT STREET NEW FARM QLD 4005 PH: 07 3254 9100 – FAX: 07 3358 4781 EMAIL:
ENQUIRIES.NFC@RAMSAYHEALTH.COM.AU WWW.NEWFARMCLINIC.COM.AU
